|
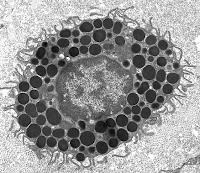
| Hookworm |
In November of 2010, a study was conducted by researchers Endara, Vaca, Chico, Erazo, Oviedo, Quinzo, Rodriguez, Lovato, Moncayo, Barreto, Rodrigues and Cooper from the Colegio de Ciencias de la Salud at the Universidad San Francisco de Quito and published in the Journal of the British Society for Allergy & Clinical Immunology. The study focused on the effect of anti-helminth treatments on the prevalence of allergies. Helminths are parasitic worms that need the resources of a host body to survive. Researchers have been experimenting with helminth therapy or the intentional inoculation of patients with helminths, for quite some time now. The theory behind helminth therapy is that our body's immune system is naturally regulated by the presence of these helminths. As part of their survival, these parasites down-regulate the part of the host's immune system that is also responsible for the auto-immune and allergic responses. However, modern society has become so "clean" that many of these parasites can no longer survive. Some theorize that the lack of natural parasites has screwed up the immune system, resulting in an increased incidence of auto-immune diseases and allergies.
Obviously there are many helminths that are so dangerous that their presence would threaten our health, but some are relatively safe. For example, low concentrations of hookworms and whipworms are not considered a real health hazard. Therefore, these "weaker" helminths have been experimented with in helminth therapy. By introducing hookworms or whipworms into patients with auto-immune diseases and severe allergies, the immune system may work itself out. In the case of allergies, this means that the body will no longer respond to an allergen. For example, the binding of pollen to the IgE antibody will no longer activate the mast cells and induce the release of histamine and other mediators. In other words, the body becomes desensitized to the allergen.
 |
| Whipworm |
In the study, researchers performed an allergen skin test on school-aged children from two different communities, to determine their reactivity to the allergen. The children of one community received the anti-helminth treatment, ivermectin, for fifteen to seventeen years, while the children of the other community did not. The researchers found that twice as many children receiving ivermectin experienced an allergic response to the skin test (16.7%), compared to the children who hadn't received anti-helminth therapy (8.7%). For children treated with ivermectin, the results show a statistically significant increase in the number of those with allergies. However, it is unclear whether other factors were accounted for. For example, the incidence of second-hand smoke or pollution may have been greater in the community giving ivermectin treatments, which may have accounted for the increased incidence of allergies in the population. Either way, helminth therapy will definitely prove to be very controversial.
Where do we drawn the line? Helminth therapy may reduce the severity of auto-immune diseases and allergic reactions, but is the danger associated with helminth therapy worth the risk? More research needs to be done, especially on the long-term risk of using this treatment. However, if helminth therapy does prove to be effective and safe in the long run, are people really going to be willing to infect themselves with a parasite? Only time will tell whether helminth therapy will become the new treatment or fade from view.
For more information about Helminth Therapy Click Here
For a more in-depth look at using parasites, take a look at the blog Waiting For The Cure, which chronicles one person's use of parasitic worms to treat Crohn's Disease
To view a Live Science article about Helminth Therapy Click Here